

A 34-year-old woman with Fanconi anemia (FA) and oral dysplasia presented to the UCSF Head and Neck Surgery Cancer Program with mucosal changes involving the tongue and mandibular gingiva. Biopsy confirmed invasive squamous cell carcinoma (SCC), and imaging demonstrated bony invasion of the mandible.
“We typically don’t see this type of cancer in such young patients, so this was certainly a manifestation of Fanconi anemia,” said UCSF head and neck surgeon Ilya Likhterov, MD. This rare autosomal recessive genetic disorder is characterized by bone marrow failure and an increased risk of certain cancers, including head and neck (HN) SCC.
“Scans showed destruction of the mandible, so we recommended composite resection, which involves resecting the segment of the mandible containing the tumor along with the surrounding oral mucosa. The resulting wound requires complex reconstruction.”
Computer-guided surgical planning enables precision reconstruction
Using computer-guided surgical planning, the UCSF team developed a detailed virtual model of the patient’s mandible to optimize surgical precision and postoperative symmetry. A patient-specific titanium reconstruction plate was fabricated preoperatively, allowing for anatomic realignment during mandibular reconstruction.
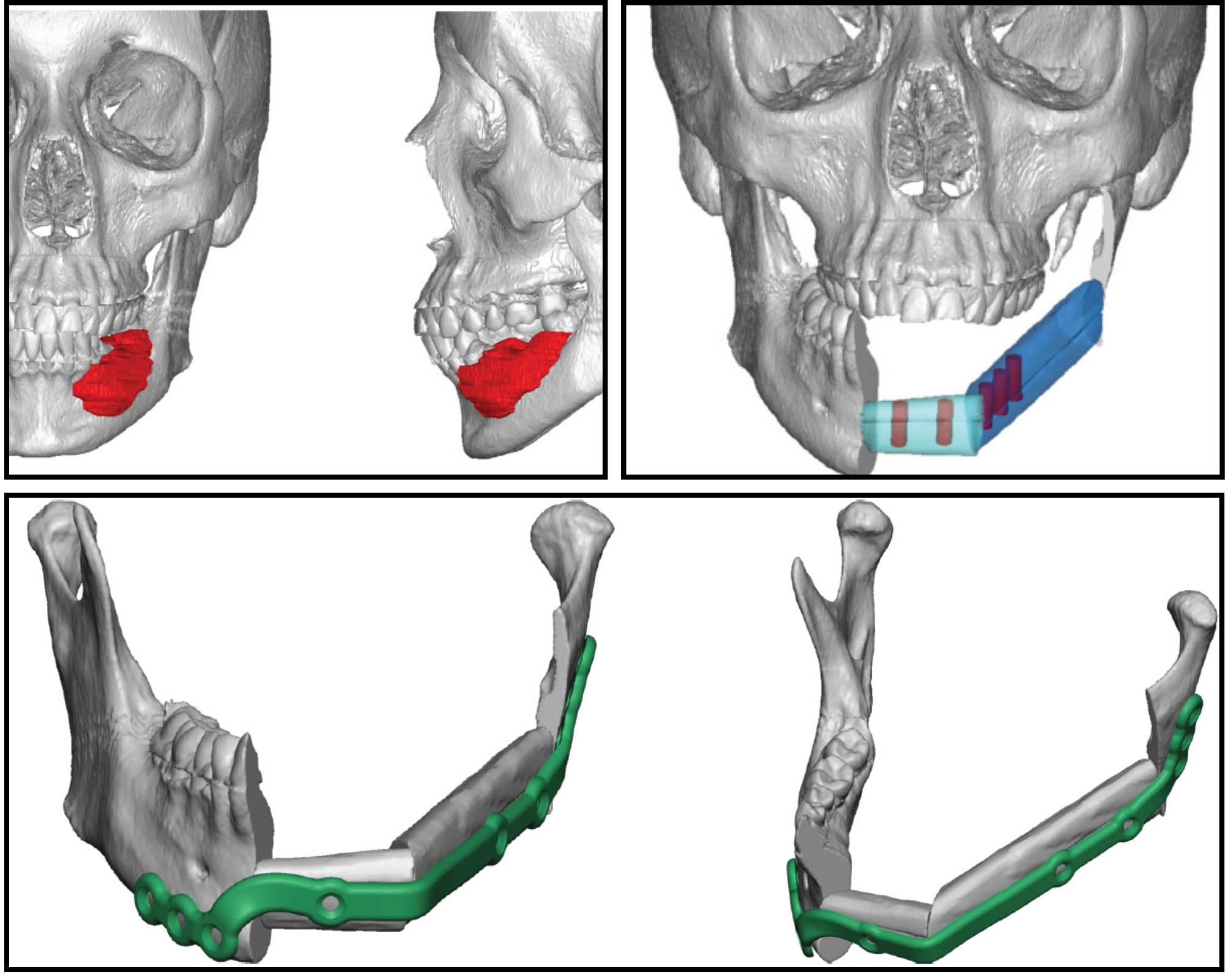
The surgical team performed a segmental resection of the left mandible – from the angle through the contralateral parasymphysis – followed by fibula free flap reconstruction with microvascular anastomosis. Dental implants were placed into the fibula graft intraoperatively in collaboration with two other UCSF specialists, an oral surgeon and a prosthodontist.
“We were able to get all of this done for her in one day thanks to the team we have here at UCSF,” Likhterov said. The patient’s oncologic care team includes head and neck cancer surgeons, reconstructive surgeons, and radiation and medical oncologists. Her functional recovery will involve speech and swallowing therapy and dental restoration with a prosthodontist. Once her cancer treatment is completed, she will be under close surveillance to monitor for signs of recurrence.
Along with the multidisciplinary team’s expertise, Likhterov’s dual role as cancer surgeon and reconstructive specialist enables precision restoration of form and function essential to quality of life for patients.
Groundbreaking patient-centered research
UCSF is one of the few centers conducting translational research specific to FA-associated HNSCC. In their lab, otolaryngologist Jennifer Grandis, MD, and Daniel Johnson, PhD, have developed four patient-derived xenograft (PDX) models from FA-HNSCC tumors to identify predictive biomarkers that may lead to novel treatments.
“To our knowledge, these are the only PDX models in the world made from FA-HNC tumors,” Grandis said.
Likhterov’s research focuses on quality-of-life outcomes following major head and neck reconstruction. He examines how various surgical techniques impact speech, swallowing and overall recovery. Previously, he was part of a team that developed and validated a patient-centered functional outcomes instrument for patients with HNC.
High-volume center for complex cases
The coordinated multidisciplinary team of specialists at the UCSF Head and Neck Surgery Cancer Program provides advanced, personalized care for patients with complex conditions, including those associated with rare genetic disorders.
“Being at UCSF means being surrounded by people doing groundbreaking work,” Likhterov said.
“Everyone on the team is performing at the highest level. Knowing that our patients are receiving the best possible care – not just from me but from the entire institution – is incredibly fulfilling.”
Cancer research and treatment take place within the UCSF Helen Diller Family Comprehensive Cancer Center.
To learn more
UCSF Head and Neck Surgery Cancer Program
Phone: (415) 885-7528 | Fax: (415) 885-7711


